Fluorescent in situ Hybridization (FISH) for Hematological Malignancies and Solid Tumors
 Fluorescent in situ hybridization (FISH) is a technique that utilizes hybridization of fluorescein labeled DNA probes to specific chromosomal regions to detect specific chromosome abnormalities. The abnormalities may be translocations, deletions, inversions, trisomies or amplification. The power of these probes results from the fact that analysis can be performed on interphase nuclei, facilitating the analysis of many more cells providing details concerning percentages of cells that are positive or negative for the rearrangement.
Fluorescent in situ hybridization (FISH) is a technique that utilizes hybridization of fluorescein labeled DNA probes to specific chromosomal regions to detect specific chromosome abnormalities. The abnormalities may be translocations, deletions, inversions, trisomies or amplification. The power of these probes results from the fact that analysis can be performed on interphase nuclei, facilitating the analysis of many more cells providing details concerning percentages of cells that are positive or negative for the rearrangement.
INDICATIONS:
- Rapid detection of specific translocations (turnaround time 24-48 hours)
- Gene amplification can be detected
- Assessment of minimal residual disease following treatment or bone marrow transplant
- Confirmation of rearrangements difficult to detect on karyotypes
- Results can be obtained in absence of dividing cells following treatment
- Detection of an early relapse Identification of the lineage of neoplastic cells.
SAMPLE REQUIREMENTS:
FISH studies can be performed on the same sample submitted for chromosome analysis. No additional sample or bone marrow is required.
FISH studies can also be performed on paraffin embedded tissue of excised tumors.
INTERPRETATION:
The diagnosis, type of sample and probe used will determine the number of interphase nuclei or metaphase spreads analyzed by routine laboratory protocol.
RESULTS:
Results are presented according to the International System for Human Cytogenetic Nomenclature (ISCN). Full explanation of the abnormality is provided and a short summary is written for each result.
FISH PROBES AVAILABLE FOR TESTING:
CANCER PROBE
CEPX/CEPY BM Transplant |
HEMATOLOGIC DISORDERS, Most Commonly Associated Diseases
Myelodysplastic Syndrome (MDS) and/ or Secondary Acute Myeloid Leukemia (AML) |
EGR1, 5q31 deletion |
EGFR, 7p12 deletion |
D7S486, 7q31 deletion |
CEP 8, trisomy 8 |
D20S108, 20q12deletion |
Acute Myeloid Leukemia (AML) |
RUNX1T1/RUNX1, t( 8:21 )(q22;q22) (M2) |
KMT2A (MLL) BA, 11q23 rearrangement (M5) |
CBFB BA, 16q22 inversion |
RARA BA, 17q21 rearrangement (M3) |
Chronic Myeloid Leukemia (CML) |
BCR/ABL df, t( 9:22 )(q34;q11.2) |
Acute Lymphoblastic Leukemia (ALL) B-Cell |
Triple Trisomy, 4, 10, 17 |
CDKN2A, 9p21 deletion |
BCR/ABL df, t( 9:22 )(q34;q11.2) |
KMT2A (MLL) BA, 11q23 rearrangement |
ETV6/RUNX1, t( 12:21 )(p13;q22) |
Acute Lymphoblastic Leukemia (ALL) T-Cell |
ABL amplification, BCR/ABL df |
CDKN2A, 9p21 deletion |
Multiple Myeloma (MM) |
1q21/8p21 gain/deletion |
Trisomy 5p15.2, 9cen, 15cen |
D13S319, 13q14.3 deletion |
RB1, 13q14 deletion |
TP53, 17p13.1 deletion |
CCND1/IGH, t( 11:14 ) |
Subtypes : IGH/MAF, t(14;16) |
FGFR3/IGH, t(4;14) |
Chronic Lymphocytic Leukemia (CLL) |
ATM, 11q22 deletion |
TP53, 17p13.1 deletion |
CEP 12, trisomy 12 |
D13S319, 13q14.3/13q34 deletion |
TP53, 17p13.1 deletion |
MYB/CEP6, 6q22-23 deletion |
B-Cell Lymphoma |
MYC BA, 8q24 |
IgH BA, 14q32.3 |
MALT1 BA, 18q21 |
BCL2 BA, 18q21 |
Subtypes: t(8;14) Burkett |
t(11;14) Mantle Cell |
t(11;18) Malt/ Marginal Zone |
t(14;18) Follicular |
Anaplastic Large Cell Lymphoma |
ALK BA, 2p23 ALCL |
SOLID TUMORS, Most Commonly Associated Diseases |
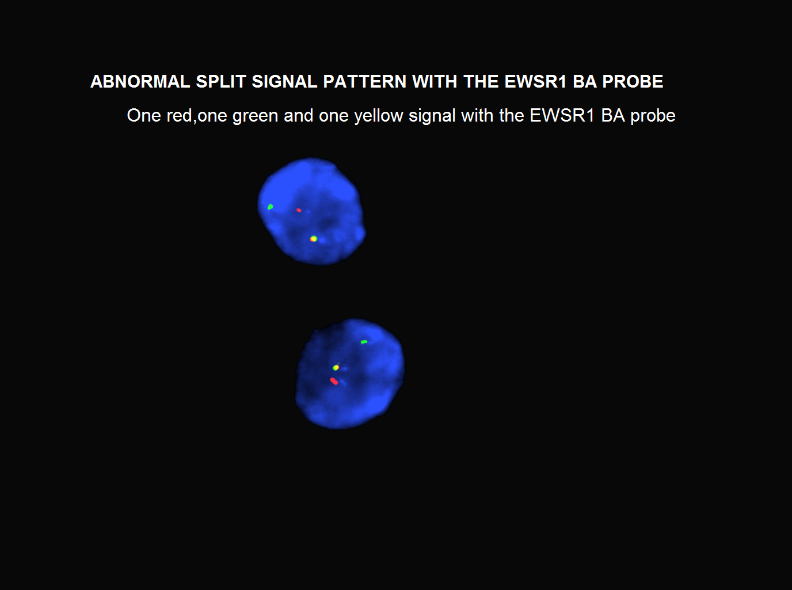
EWSR1 BA, 22q12 Ewing’s Sarcoma |
MYCN, 2p23-24 Neuroblastoma |
FOX01 BA, 13q14 Rhabdomyosarcoma |
SS18 BA, 18q11.2 Synovial Sarcoma |
RB1, 13q14 deletion Retinoblastoma |
Cyclin D1, 11q13 head, neck & breast cancer |
DDIT3 BA, 12q13 Myxoid Liposarcoma |
FUS BA, 16p11 LGFMS & MLS |
TP53, 17p13.1 Li-Fraumeni syndrome |
ALK BA, 2p23 Inf. Myofibroblastic and lung cancer |
Her2neu, PathVysion, 17q11.2 Breast Cancer |
TFE3 BA, Xp11 |

 Institute of Genomic Medicine
Institute of Genomic Medicine